Leiden researchers grow mini-skeletal muscles for FSHD muscle disease research
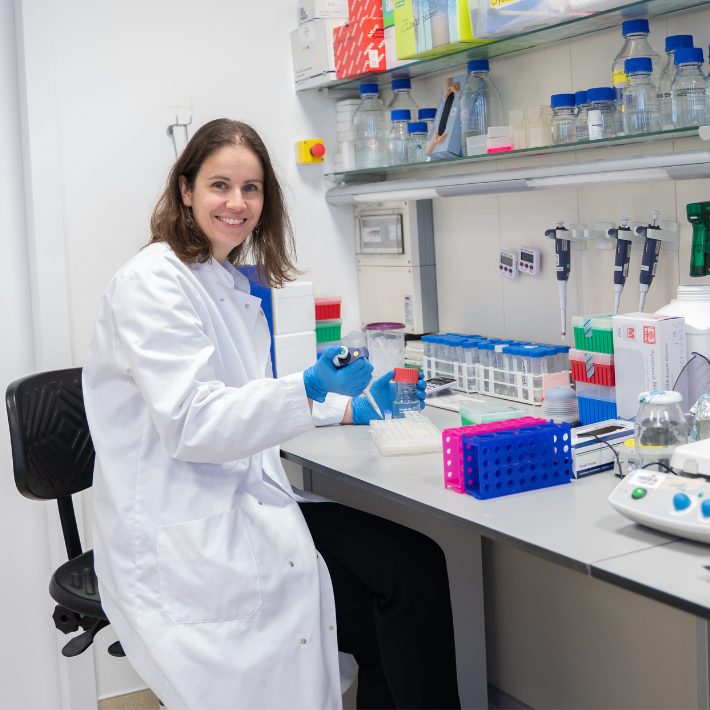
FSHD researcher Dr. Jessica de Greef. (Source photo: Spierfonds)
&width=710&height=710)
Currently, there are no therapies for FSHD, full name facioscapulohumeral muscular dystrophy. The muscle disease is very rare. It is estimated that there are about 2,000 patients in the Netherlands and 500,000 worldwide. Nevertheless, FSHD is one of the most common hereditary muscle diseases. The LUMC is a center of expertise in the field of FSHD and excels worldwide in research into the disorder.
FSHD is characterized by muscle weakness that usually begins in the face: facial expression diminishes. The disease is progressive, meaning the symptoms keep getting worse. In some patients this progresses very slowly, so the symptoms remain mild. About 1 in 5 patients lose the ability to stand up and walk and may become wheelchair dependent.
Testing mini-muscle strength
To research possible new drugs for FSHD, mini-muscles are grown in the laboratory. For this purpose, skin cells were taken from three different FSHD patients. From these skin cells stem cells are made, and from these stem cells muscle cells, from which muscle fibers are then made.
Until recently, researchers only had the ability to grow a flat layer of muscle cells (in two dimensions). With the new method, miniature muscles grow in a 3D structure. As a result, researchers can now also measure muscle strength. “We let those 3D muscles grow for at least a week in a culture box between two pillars. They do that largely by themselves, just as they would do in the body between two tendons,” says FSHD researcher Dr. Jessica de Greef.
Then it's time to test the strength of the mini-muscles. This is done through electrical stimulation that causes the muscles to contract. “The muscles are attached to the pillars. The pillars have a certain flexibility. When the muscles contract, they can make the pillars bend. From there we can calculate exactly how strong the muscle is. This makes the models very suitable for drug testing,” she says.
Fewer laboratory animals
The researchers also hope that with the 3D models, fewer laboratory animals will be needed to test on. “We can be more selective in test animal use. Because suppose you know something doesn't work on 3D muscles, you don't need to continue testing in mice, for example. The same eventually applies to studies with human subjects. In that, too, we have to be very selective. There are only about two thousand FSHD patients in the Netherlands. Suppose you can find a hundred who want to participate in a drug study, then those hundred people cannot participate in another drug study. In other words, we have to make sharp choices: what are we going to test and what not? These kinds of 3D models help with that,” says De Greef.
Mosaic patients
The FSHD cells that the researchers used to make 3D muscles came from three so-called mosaic patients. “In these individuals, a mutation (change in hereditary material) occurred during cell division in the early embryonic stage. Some body cells have the mutation and others do not. The advantage for us is that we can compare healthy and diseased cells from the same patient.”
Muscles made from the diseased cells showed symptoms that clearly matched those of FSHD patients. Such as reduced contraction forces (the contraction of muscle tissue) and thinner muscle fibers and shorter sarcomeres (tiny particles in the muscle that help make the muscles work).
The findings were published in the scientific journal Brain.
Video: Menselijke spiertjes maken in het spierziektenlab
&width=710&height=710)
&width=710&height=710)
&width=710&height=710)
&width=710&height=710)