Cancer therapy with engineered immune cells significantly reduced
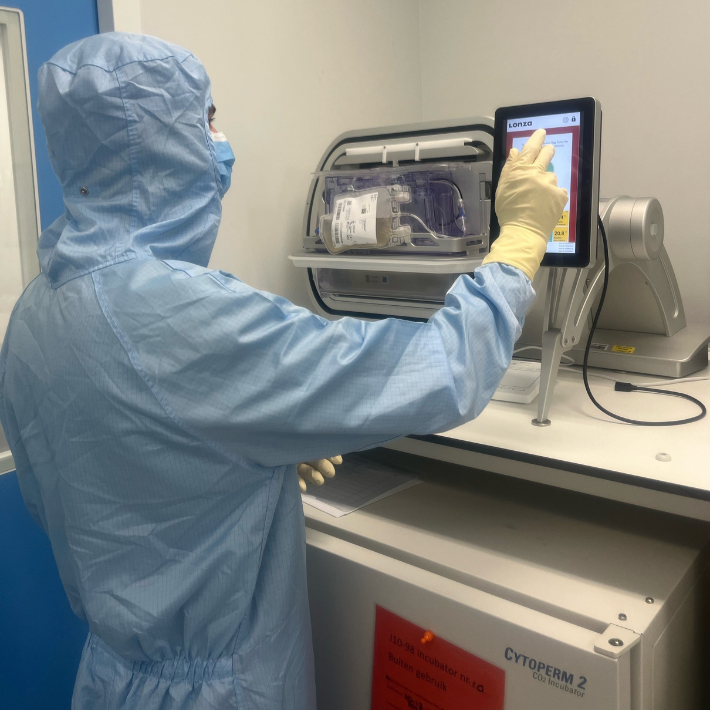
An analyst performs the final checks before the transformed immune cells will be returned to the patient. The cells have had a week to grow in the cocoon (an advanced incubator).
&width=710&height=710)
This treatment, called CAR-T cell therapy, uses the patient's genetically engineered endogenous immune cells (T lymphocytes) to fight the cancer cells. By doing that genetic alteration in LUMC's own laboratory rather than in an outside lab, the process has been dramatically accelerated.
How does CAR-T cell therapy work?
Specialists in the Department of Hematology extract T cells from the patient's blood. Then these cells are genetically altered in a laboratory so that they better recognize and destroy cancer cells. The altered immune cells are then called CAR-T cells. The patient gets those cells back by infusion. The therapy is successful: about 45 percent of patients with some form of aggressive lymphoma (who are normally out of treatment) seem to be cured thanks to the treatment. CAR-T cell therapy is therefore the biggest breakthrough in cancer treatment in recent years.
In-house laboratory
Joost Vermaat, internist-hematologist at LUMC : "Until recently, the production of CAR-T cells took place in a manufacturer's laboratory. This had major disadvantages. Sending the cells back and forth took over four weeks. Besides being time-consuming, the process was also expensive: the cost per treatment quickly ran to about 500,000 euros. In addition, the exact composition of the product was known only to the pharmaceutical company, which could lead to uncertainty about the quality for both patient and physician."
"Since we can now produce these CAR-T cells ourselves, we can treat a patient within a week. Also, the costs are significantly smaller. Another advantage is that we know exactly how many and which cells are returned to the patient. The latter also provides insight on how we can potentially improve the therapy even further," says researcher and head of the production lab in the hematology department, Rosa de Groot.
Ten patients in the LUMC have now been successfully treated with self-prepared CAR-T cells. Treatments of other patients are on the schedule for the coming months. These treatments are being done in trials (including Atalanta). The in-house CAR-T cell production uses the skill of the lab and good cooperation between a range of departments*.
Side effects
"Yet there are also downsides to CAR T cell therapy," Vermaat said. "The treatment is intensive and all patients suffer from side effects. Usually these are well treatable, but occasionally the side effects are so severe that the patient ends up in intensive care. Fortunately, developments in this new form of treatment are advancing rapidly. We are aiming to increase the effectiveness, reduce side effects, develop new CAR-T products for other types of cancer and make healthcare cheaper by manufacturing it ourselves. An ambitious target, but we are confident."
At LUMC, the department of hematology is continuing the development of CAR-T cell therapy. They are doing this in collaboration with the Cellpoint/Galapagos company. This also includes other diseases, such as chronic lymphatic leukemia and multiple myeloma (Kahler's disease).
* CAR-T cell production at LUMC is based on cooperation between the departments of radiotherapy, neurology, cardiology and intensive care, pharmacy and the Center for Cell and Gene Therapy.