Coloscopie (English) (MDL)
Endoscopy department for gastrointestinal and liver diseases
Wat is Coloscopie (English) (MDL)?
What is a colonoscopy?
A colonoscopy is a visual examination of the intestines to find the cause of your complaints. The doctor will use an endoscope for this examination. This is a flexible tube with a camera and a light in it. If you have abnormalities in the colon, treatment may be possible.
Hoe kunt u zich voorbereiden?
Preparation fort he examination
Clothing
Wear comfortable, non-constricting clothing. Jewelry or other valuables can be lost. It is therefore better to leave them at home.
Medicines
Some drugs affect the examination and treatment. Therefore, please follow the instructions below.
Anticoagulation
If you use blood thinners (such as; Ascal, Plavix or the new anticoagulants),
report this to your treating doctor.
The doctor will then determine whether the blood thinner can be temporarily
stopped. If you use a blood thinner that the Thrombosis Service checks (such
as phenprocoumon, marcoumar or acenocoumarol), the Thrombosis Service
must adjust the dose. In that case, you must contact the Thrombosis Service as
soon as the date of the examination is known. An INR determination is
required on the day of the examination and will be tested in the hospital prior
to the examination.
Glucose Controlling Drugs
If you have diabetes mellitus, you will receive advice from your attending
physician about adjusting your blood sugar-regulating medication. If in doubt,
please contact your diabetic nurse. You can also find information on this
subject in the patient folder ‘Coloscopie en diabetes mellitus, instructie
bloedsuikerverlagende medicijnen’.
In general, you can take your other medicines in the usual way and at time.
Report particularities in advance
Let us know if you have a physical disability or handicap. Then, if necessary, we can schedule extra time for the procedure.
Unable to attend procedure?
Let us know, on time, if you are unable to attend at the procedure so we can reschedule and use the time slot to help another patient.
Hoe gaat het onderzoek / de behandeling in zijn werk?
Preparation schedule and diet
For this examination it is very important that the colon is completely empty
(clean). If there is still stool in the intestine, abnormalities (e.g. polyps) can be
missed. In some cases, the entire examination (including preparation) must be
redone. Therefore, follow the instructions below very carefully.
You will be given a prescription for laxative fluid (Pleinvue®, Moviprep® or Klean prep®) and laxative pills (Bisacodyl®). Read the attached leaflet about the bowel preparation carefully and follow the diet and preparation schedule step by step.


Contaminated bowel (poor vision) Clean bowel (good vision)
Day of procedure
Where should you report yourself?
The examination is performed on an outpatient clinic basis in the Endoscopy Department. You can register at the entrance of the hospital at the registration column. You will receive a ticket from the column. The hostesses/men in the central hall are happy to show you the way. You can sign in at desk 119, route 170 (C04-S). The department is located on the fourth floor of the hospital building. Due to some pre-procedural preparations, you must be present 30 minutes before the examination starts.
Colonoscopy with sedation
The examination is performed with a sedative (sedation). Sedation is not an
anesthetic but a relaxant. The sedation can make you sleepy and help you relax during the examination.
Accompaniment
As you will receive sedation for this examination, it is necessary that someone
picks you up from the Endoscopy Department, C04-S, route 170. You are not
allowed to go home alone, not even by public transport or taxi. You are not
allowed to drive a vehicle all day and it is wise to take it easy and not to work
for the rest of the day.
Please note: if you have not arranged transport back home, the examination cannot take place.
The colonoscopy
Prior to the colonoscopy an IV needle will be placed for medication during the colonoscopy.
The endoscopy nurse will take you to the examination room and will ask some
questions to check. During the examination you will lie on your left side or on
your back. You get a 'pincer' on your finger. We use this pincer to monitor your heart rate and blood oxygen level during the examination. Also we will connect you to a blood pressure band for blood pressure measurement and administer the sedatives and painkillers through an IV needle.
Before the procedure starts a couple of questions will be asked, this is called a Time-Out Procedure.
The endoscope is coated with gel and inserted through the anus. Pushing the
hose in can sometimes cause an unpleasant feeling. During the examination,
the doctor will blow some air through the endoscope into your bowel for
better sight. However, this can give you a bloated feeling and it is
recommended to just let wind pass during the examination. Also after the
examination the urge to fart is very normal and relieves you from the bloated
feeling. In some patients, moving the endoscope is more difficult because the
colon is very tortuous. It is best if you try to relax during the examination. The
nurse will give you instructions for this.
The doctor can remove some tissue from the inside of the intestine using a thin
forceps. This is called a biopsy. You will not feel this. This tissue will be further
examined under the microscope. Treatment will be performed, if necessary.
Sometimes people still have pain or feel unwell right after the procedure. If this is the case, tell the nurse and/or doctor.
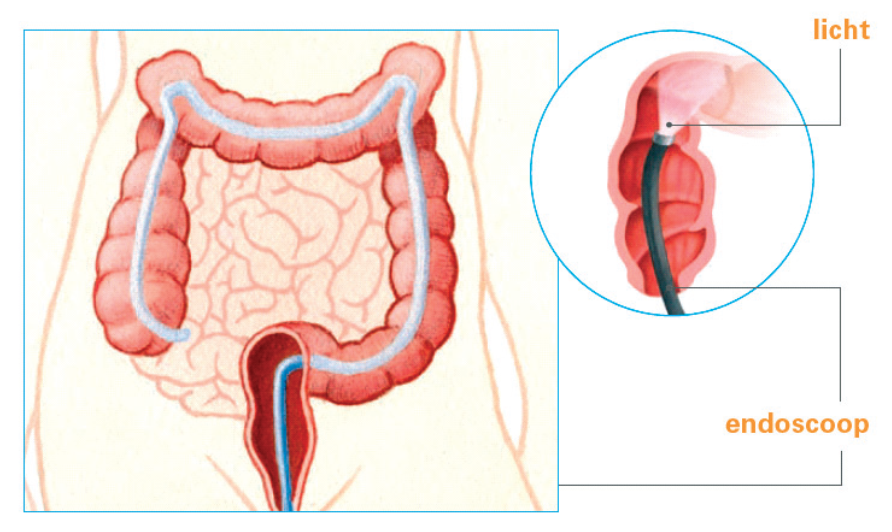
In the picture above you can see how the endoscope works. The endoscope
bends along with the shape of the large intestine. The light at the end of the
endoscope allows the doctor to see the inside of the colon.
Duration of the procedure
The examination takes approximately 45-60 minutes.
Waar moet u op letten direct na het onderzoek / de behandeling?
After the colonoscopy
If you are admitted to hospital, you will immediately return to the ward.
Otherwise, you will remain in the recovery room for another 15 to 30 minutes.
After observation in the recovery room, you must be picked up from the
Endoscopy Department and you can go home with your companion.
If you have received deep sedation (propofol), it is necessary that someone is with you during the night. See patient leaflet ‘Deep sedation (propofol) for
endoscopy’.
Wanneer krijgt u de uitslag?
Results
You will receive a preliminary result or a report of the examination to take
home. You will receive the final results later, at your follow-up appointment at
the outpatient clinic.
Wat zijn de risico's, bijwerkingen of complicaties?
Risks and side effects
In general, a colonoscopy is a safe procedure. There is a very small chance
(less than 0.1%) of a complication. Complications that can occur are a bleeding
or perforation (hole in the intestines). If we notice a complication during the
endoscopy, we try to treat it right away. In some cases, you will need to be
hospitalized after the endoscopy and surgery may be required.
Contact bij problemen na uw onderzoek/behandeling
Do you have any questions?
If you have any questions, you can contact the Endoscopy Department of
Gastrointestinal Liver Diseases. You can do this on working days between
8.00 – 11.00 via telephone number 071-526 31 88.
In case of medical problems, you can contact the LUMC through
telephone number 071 – 526 91 11 and ask for the gastroenterologist on duty.
In case of medical problems, such as a lot of abdominal pain or bright red
blood loss through the anus after the colonoscopy